Approximately 2% to 6% of men who’ve had a vasectomy eventually wish to regain their fertility. Although a vasectomy has long been considered an irreversible form of contraception, this is no longer the case.
If a man wishes to have children with his partner following a vasectomy, he has two options:
- A vasovasostomy (vasectomy reversal)
- Testicular sperm extraction in conjunction with intracytoplasmic sperm injection
Generally, a vasectomy reversal is the preferred option. Unlike artificial fertilization techniques, it has a high success rate and carries a low risk of complications.
Prior to the vasectomy reversal , an initial consultation at which both partners are present is conducted. The procedure itself is performed at a second appointment.
Please note that vasovasostomies are done in an unaffiliated private clinic and can’t be reimbursed through the Regie de l’assurance maladie du Québec (RAMQ).
Please note that vasovasostomies are performed exclusively in a non-participating private clinic to the RAMQ. They are not reimbursable by the RAMQ.
Is a vasectomy reversible?
The desired outcome of a vasectomy is to prevent sperm from passing through the vas deferens, which are ducts in the testicles that carry the sperm to the ejaculatory ducts. During the procedure, each duct is cut and tied. As a result, the ejaculate no longer contains any sperm and the unused sperm gradually degenerates.
During a vasovasostomy the severed segments of the vas deferens are reconnected. Sometimes, the procedure is not possible for anatomical reasons. In such cases, the vas deferens can instead be connected directly to the epididymis (a tube at the back of the testicles that stores the sperm produced by the testicles). This operation is called a vasoepididymostomy and is more technically complex than a vasovasostomy.
What are the factors insuring an optimal surgical technique?
- Number of layers or closure planes: It is well recognized that the success rate of repairing canals in 3 planes (mucosa, muscularis and adventitia) is much higher than repair in 1 plane. This explains the considerable length of this surgery.
- The precision of the surgical microscope: a good microscope will allow better magnification, better stability and adjustable focus. It will therefore allow for greater precision of the image and the sutures at the different layers of closure. Furthermore, it is well recognized that this surgery performed with magnifying surgical loupes is an outdated and suboptimal technique.
- Observation of the differential fluid by a 2nd microscope during surgery: this provides assurance that the canal is not obstructed. If there are no sperm fragments, the duct will be cut further down, sometimes even to the point of making a vasoepidimostomy.
- Canal repair site reinforcement and support technique: in order to provide tension on the repair site and to reduce the risk of dehiscence of the anastomosis.
- Surgical skill, if a vasoepidimostomy is necessary: the probability of performing it increases depending on the number of years of vasectomy. This technique is more difficult in some cases, since the incision must be extended to expose the epididymis, removing part or all of the testicle. Dr Marois has more than 200 reversals to his credit with an excellent success rate. Dr. Gagnon was trained by Dr. Goldstein at the prestigious Cornell University and benefited from the mentorship of Dr. Marois.
- Experienced nursing staff: surgery being a team effort, the staff who are used to attending this surgery are able to give pre and post-operative recommendations, to carry out appropriate nursing follow-ups, to reassure patients, to recognize particularities requiring the opinion of the urologist.
- Knowledge of laboratory interpretations for testicular function: the fertility of certain men may decrease with age and certain particularities may require specific laboratory tests. Certain hormonal interventions may also be necessary to help fertility.
What’s the success rate for a standard vasectomy reversal?
- It’s important to understand that a vasectomy is meant to be irreversible, so there’s no guarantee that a patient’s vasectomy reversal will be successful.
- Various factors influence the probability of achieving a pregnancy after a vasectomy reversal. One of the most important factors is the reproductive potential of the man’s partner. Women under 30 are generally more fertile than older women. Among couples trying to have a baby following a vasectomy reversal, pregnancy occurs 14% of the time when the woman is over 40, 56% of the time when the woman is aged 25 to 39, and 67% of the time when the woman is aged 20 to 24.
- The most important factor for men is the time between the vasectomy and the vasectomy reversal.
- The success rate is based on the patency rate. This refers to the percentage of men who have sperm in their ejaculate following the procedure. The patency rate after a vasectomy reversal is about 75% to 85%. Our urologists verify the presence of sperm in the vas deferens during the surgery, in order to know if he will reconnect the ends of the vas deferens together, or go further in the epididymis.
- If complications from the vasectomy resulted in a significant amount of scar tissue, it can reduce the chances of the vasectomy reversal succeeding. Trauma or infection of the scrotum can also reduce the success rate.
- In some cases, the patient isn’t able to produce sperm following the surgery. Alternatively, he may produce what are known as antisperm antibodies, which can make it harder for a couple to have a baby.
- Note, also, that a vasoepididymostomy has a much lower success rate than a vasovasostomy (around 30% to 45%).
- Finally, the surgeon’s degree of experience is essential to the success of the operation : this directly relates to the number of vasovasostomies a surgeon performs per year. Dr Marois does about a hundred every year, and has done so for the last 10 years using the best technology.
What are the chances of pregnancy after a vasectomy reversal?
When the interval between the procedures surpasses 15 years, the patency rate is 70% and the pregnancy success rate is 30%. This lower success rate is primarily since, as time passes, the narrow, coiled tube of the epididymis becomes increasingly at risk of incurring damage. This damage is mainly the result of pressure resulting from the constant buildup of fluids and sperm produced in the testes. Although this doesn’t always cause visible damage, scar tissue may form at the site of the epididymal rupture and present an additional obstacle in the path of the sperm.
Another statistic from a study in the Canadian Urological Association Journal (November 2007, Vol. 1, No. 4, pp. 388-393) evaluating the success factors for a vasovasostomy clearly demonstrated a progressive decrease in the patency rate and the pregnancy success rate relative to the interval of time between the vasectomy and the vasovasostomy.
Does the age of the patient influence the success rate?
What are the possible complications after a vasectomy reversal?
There is no influence on the patient’s sexuality.
How long to become pregnant after a vasovasostomy?
However, it’s important to note that it may be more difficult to get a partner pregnant after a vasovasostomy than it was in the time prior to the vasectomy. Specifically, this is the case when (a) fibrosis in the vas deferens or epididymis is extensive, (b) the quality of patient’s sperm has degraded, or (c) antisperm antibodies are present in the patient’s ejaculate. As a general rule, a man’s reproductive potential after a vasovasostomy is weaker than it was prior to the vasectomy.
What can you do to improve semen quality after a vasectomy reversal?
Our patients are also encouraged to steer clear of medications that can degrade semen quality, such as H1 antagonists (used as treatment for gastric ulcers, among other conditions), antibiotics of the macrolide and nitrofuran family, anti-epileptics (valproate), anti-retrovirals (Salazopyrin), ketoconazole (Nizoral) and colchicine. Furthermore, most testosterone supplements should be given a miss.
If possible, you should also avoid periods of abstinence. Numerous studies indicate that the sperm become less fertile when the man has not engaged in sex for more than three days.
Another thing to remember is to not allow the testicles to have repeated and prolonged exposure to high temperatures. Testicles are meant to have a temperature of around 35°C; higher temperatures can degrade semen quality. This fact is especially relevant to cooks, bakers, metalworkers, truck drivers and other individuals whose work exposes them to heat. Note also that a high fever can cause a significant and prolonged drop in sperm production (for about 2 to 3 months).
Other things to avoid: hot baths, tight-fitting underwear and pants, and placing your computer on your lap.
Exposition of the perineum or testicles to microtrauma: avoid activities such as mountain biking, ATV riding and horseback riding.
Taking multivitamins. Certain products have been shown to increase the reproductive potential of men with abnormal sperm. Products with antioxidant properties, such as vitamin C, vitamin E, Zinc, Selenium and Folic acid can improve semen quality. Taking a vitamin supplement that includes all these ingredients is generally a good idea.
One good option is PROfortil, a multivitamin containing 18 vitamins and minerals that work together to improve semen quality. It’s frequently used in fertility clinics. Moreover, 5 European studies have demonstrated its benefits. Notably, in a controlled study of 205 patients, it was shown to produce benefits across all the major parameters of semen quality: ejaculate volume, sperm count, motility and morphology. Furthermore, after only 3 months of taking PROfortil, 26% of men got their partner pregnant. This drug can only be obtained online — for example, through the Canadian website, conceptionplus.ca.
In addition, there are medications that improve semen quality. Clomid(whose generic name is clomiphene citrate) is the most used fertility drug among women; however, it also stimulates sperm production in men with low sperm motility, low sperm count and overall poor semen quality. Specifically, clomid blocks the effect of estrogen on the pituitary gland, resulting in an increase in levels of follicle stimulating hormone (FSH) and luteinizing hormone (LH). Higher levels of these hormones increase testosterone production, which, in turn, can increase sperm count and overall semen quality. Clomid comes in tablet form and the patient takes it orally every day, generally with an initial dose of 25 mg, or half of a 50 mg tablet.
Our urologists closely monitor their patients’ hormone levels to ensure that they remain within the ideal target range, as too much testosterone can decrease sperm count. It can take three to six months before sperm production is improved. Sperm analysis tests are necessary during this period. Once sperm production reaches normal levels, the treatment can be suspended.
What anesthetic is used during a vasectomy reversal?
- The anesthetic only affects the area around the injection.
- For a more effective anesthesia and more comfortable vasectomy reversal, a spermatic cord block is administered on both the left and right side. This eliminates pain inside the scrotum. We wait 12 minutes before beginning the procedure. This is the moment when the anesthetic is at its most effective.
- The fact that the anesthesia is local, results in diminished fees (as opposed to general anesthesia) and the fact it is performed in a clinic (as opposed to a public or private hospital), results in more accessible appoitments.
What can patients expect to happen during a vasovasostomy?
- For optimal comfort, the patient is laid on his back on a gel mattress. A protective screen is placed below his head to shield his view and make the operation less stressful for him. Sterile sheets are placed on the patient and on the surgical microscope.
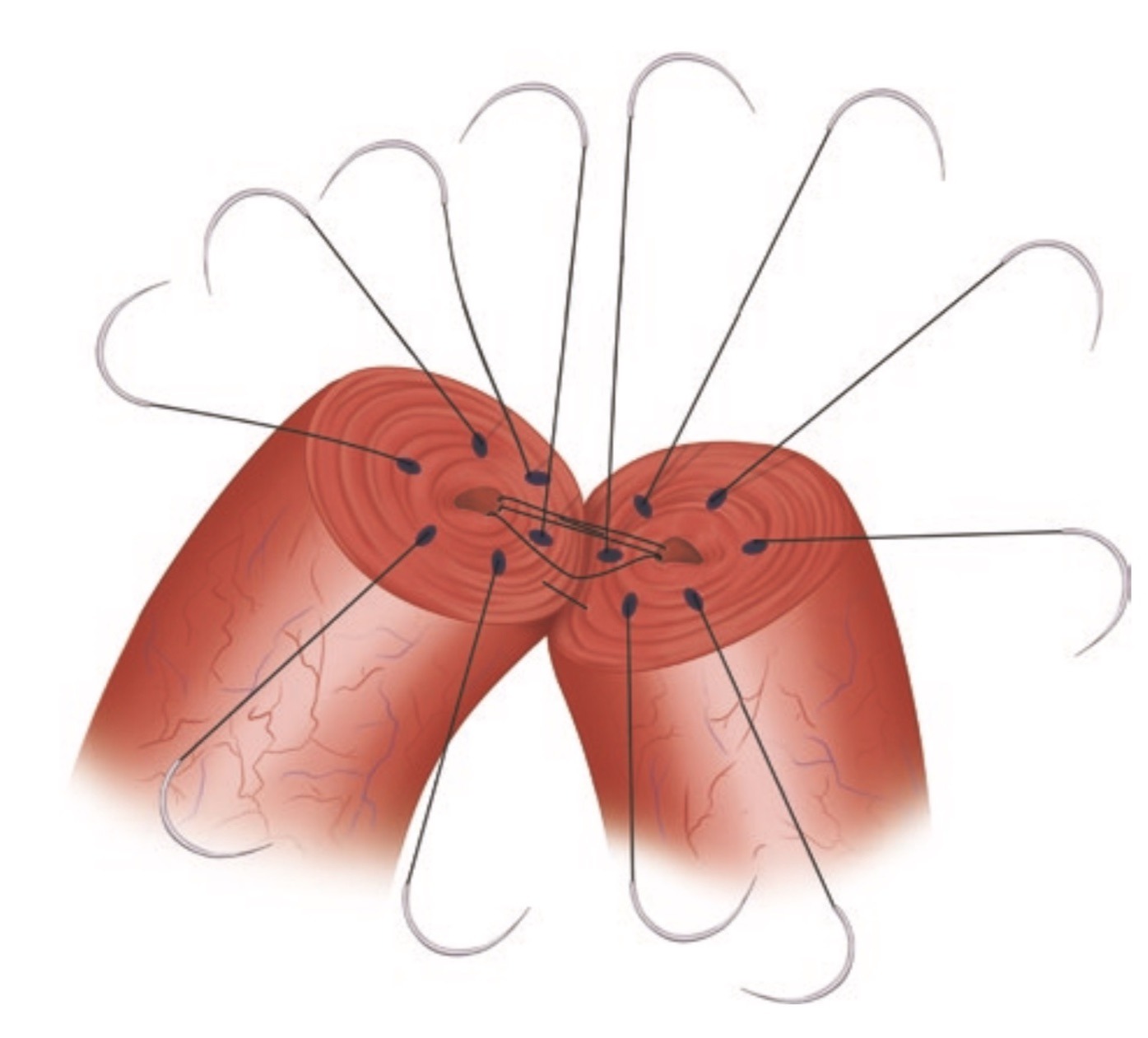
- Two incisions are made in the scrotum, on either side. The vas deferensis accessed with an incision of several millimeters (like the Chinese technique used for the vasectomy). This exposes the two ends of the vas deferens and allows their reattachment. The scar tissue on both ends of the vas deferens is removed. The urologist proceeds with the surgery, if the vas deferens is in sufficiently good condition to allow satisfactory sperm flow.
- Next, the permeability of the epididymis is verified by extracting a liquid sample and examining it under a microscope.
- The presence of sperm is then assessed in a small microscope; if judged sufficient, the urologist will proceed to reconnect the ends of the vas deferens together. However, if the presence of sperm is not deemed sufficient, he will opt to reconnect the vas deferens directly in the epididymis on both sides.
- The vasectomy reversal is performed with a high-resolution surgical microscope.
- Each vas deferens is stitched together with fine sutures, hardly visible to the naked eye. Due to its complexity, the procedure can take up to 1 hour per side (or 3 to 3,5 hours in total)
How much does a vasectomy reversal cost?
After the consultation, a surgery can be scheduled for some time within the next few weeks.
All vasectomy reversal surgeries are performed at our South Shore and Quebec clinics.
The fee for a bilateral vasovasostomycovers the use of a minor surgery room, with the assistance of one or two nurses for about 3,5 hours. It’s a microsurgery that uses very small sutures and is carried out using a high-precision surgical microscope.
Included in the price of the procedure are a telephone follow-up appointment conducted by a nurse and all needed post-operative visits (for the two months following the surgery) in the event of complications. Also included are updates with a nurse regarding the semen analysis, one at three months and one at six months after the operation.


