Condyloma Acuminatum (CA, also known as genital warts) refers to an epidermal manifestation, attributed to the epidermotropic human papillomavirus (HPV). More than a 100 types exist and many of these have been related directly to an increased neoplastic risk in men and women.
A diagnosis of CA is often distressing for men and associated with concerns regarding cosmetic appearance, stigmatization, personal health, and sexual relationships.
What are genital warts?
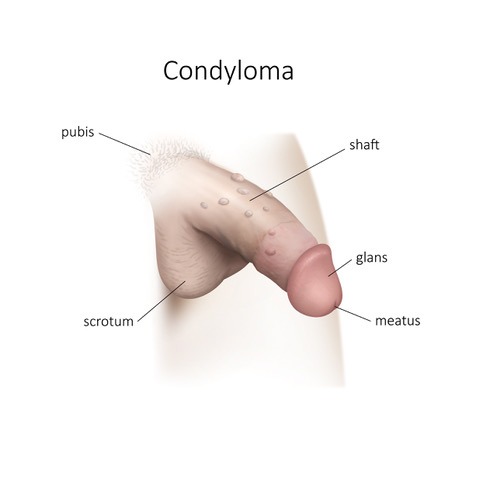
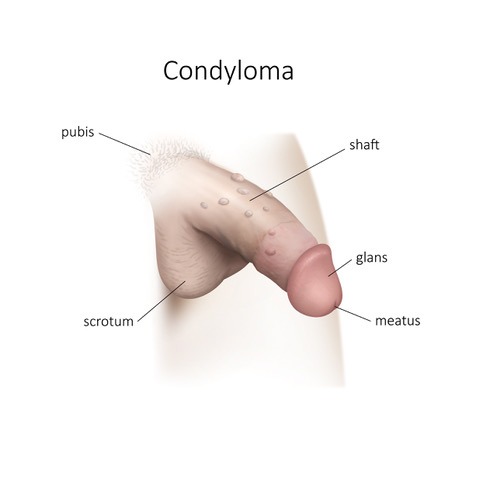
They are cauliflower-like or flat-like growths on the penis or the scrotum.
They are often multiple, asymmetrical and polymorphic.
They occur anywhere, especially in areas of friction sites (e.g., skin on skin, skin on mucous membrane, or mucous membrane on mucous membrane).
They are generally asymptomatic: itching and, more rarely, bleeding.
They are often multiple, asymmetrical and polymorphic.
They occur anywhere, especially in areas of friction sites (e.g., skin on skin, skin on mucous membrane, or mucous membrane on mucous membrane).
They are generally asymptomatic: itching and, more rarely, bleeding.
When is the surgery proposed to a patient?
Dr Marois highly recommends the surgery, if the lesions persist after medical treatment with Condyline drops, Aldara cream (to stimulate the immune system) or liquid nitrogen treatment. These treatments however, do not get rid of the HPV infection; a person who has been treated may still pass it on, even if the warts are no longer visible. Dr Marois may also offer a vaccine, if necessary.
What exactly is a fulguration or an excision of genital warts?
The procedure is done in Dr Marois's clinics. The patient receives medicine that numbs the area around the warts (local anesthetic).
First, the lesions are outlined with a marker and then disinfected.
Small lesions are burned with an electronic scalpel; this is a fulguration.
Larger lesions are removed and the skin is closed with absorbable sutures; this is an excision.
The post-operative recommendations are the same for both procedures.
First, the lesions are outlined with a marker and then disinfected.
Small lesions are burned with an electronic scalpel; this is a fulguration.
Larger lesions are removed and the skin is closed with absorbable sutures; this is an excision.
The post-operative recommendations are the same for both procedures.
References?
INESS: www.iness.qc.ca>condylomes_GUIDE_ITSS-EN
AGENCE DE LA SANTÉ PUBLIQUE DU CANADA: www.canada.ca/fr/sante-publique/services
AGENCE DE LA SANTÉ PUBLIQUE DU CANADA: www.canada.ca/fr/sante-publique/services


