What is Chronic epididymitis
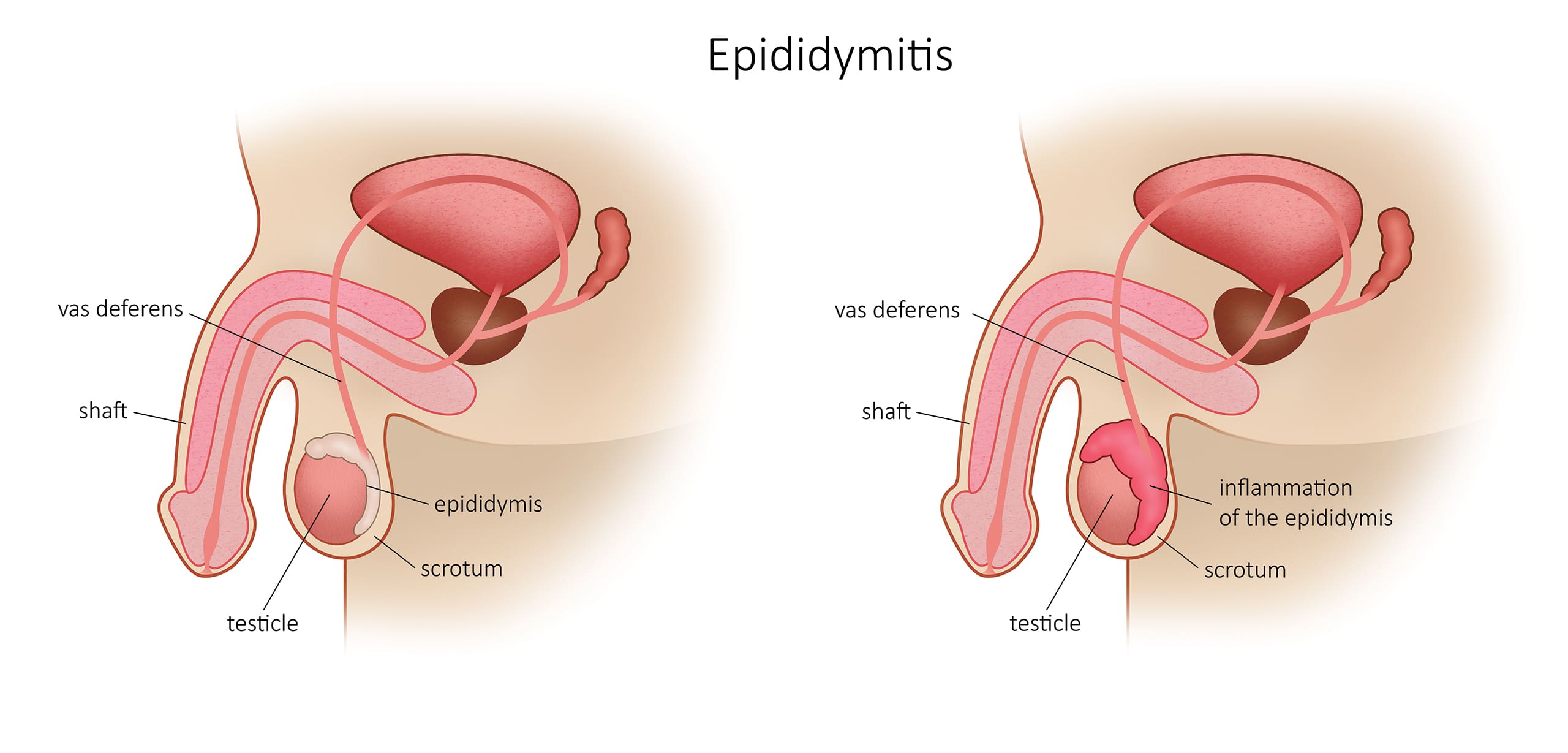
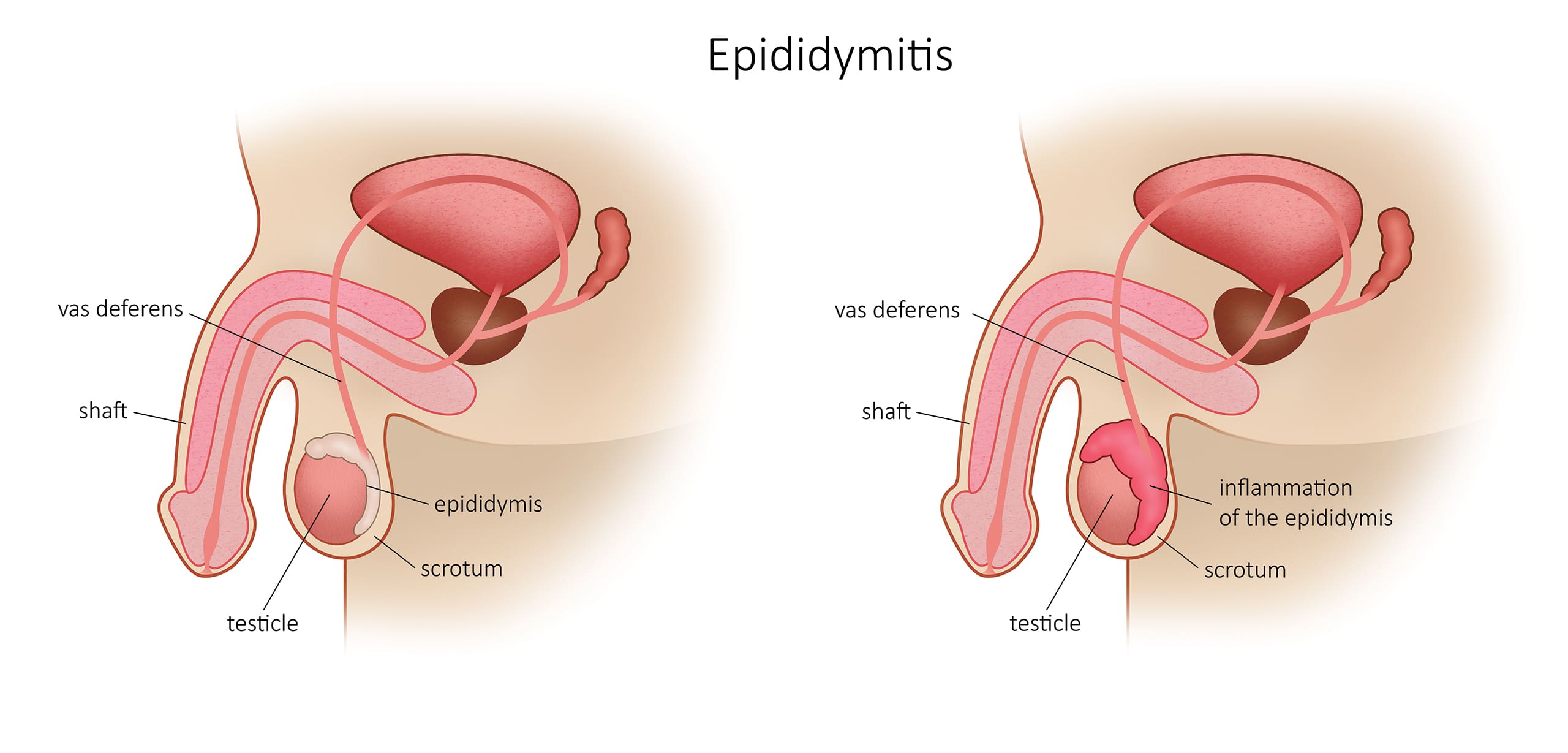
The epididymis is an elongated organ on the upper and posterior part of the testicle; it contains a duct, which receives the spermatozoa at the exit of the testicle and transports them to the vas deferens; it ensures the maturation of semen.
Chronic epididymitis is typically characterized by scrotal pain demonstrating little swelling of the epididymis for more than 6 weeks. It is usually not improved after antibiotic treatment.
What it is the cause of a chronic epididymitis?
The cause is often multifactorial and the pathophysiology is poorly understood.
Medical consensus regarding the treatment of a chronic epididymitis?
Treatments are still often based on empirical behaviour with a low level of evidence. Initial treatment of chronic epididymitis is always conservative:
- Given the difficulty of having an objective assessment of pain from one patient to another - Given that the cause is often multifactorial - Given the low level of evidence on which the indications and results of surgical treatments are based.
However, epidemic drug and non-drug treatments have been reported in the literature.
- Given the difficulty of having an objective assessment of pain from one patient to another - Given that the cause is often multifactorial - Given the low level of evidence on which the indications and results of surgical treatments are based.
However, epidemic drug and non-drug treatments have been reported in the literature.
What are the pharmaceutical treatments for chronic epididymitis?
- Nonsteroidal anti-inflammatory treatment with NSAIDs for three months before considering more aggressive treatments.
- An alpha-blocker has been proposed as a result of experimental studies.
- Tricyclic antidepressants and anticonvulsants used in the treatment of peripheral neuropathic pain are part of the treatment options.
Are there other medical treatments for chronic epididymitis?
- Adaptive and behavioral changes (limitation of physical and sexual activity, scrotal support, local ice, relaxation, yoga) have been successfully applied in a small number of patients.
- Biofeedback techniques, acupuncture and psychotherapy may also have a place in the management of chronic pain.
- Transcutaneous Electrical Nerve Stimulation (TENS) is a non-pharmacological therapeutic option validated in the management of chronic pain. The nursing staff will be able to supervise the first trial and propose rental solutions of the device for home treatments.
- An infiltration of the spermatic cord is sometimes a compromise solution.
What are the surgical treatments for chronic epididymitis?
- Surgical options described in the literature include epididymectomy, orchiectomy, vasovasostomy, and microsurgical denervation of the spermatic cord. There are no randomized controlled trials to compare these different procedures with each other, but the epididymectomy is the simplest solution.
- Orchiectomy is proposed by some as a gesture of last resort in cases of irreducible pain after medical treatment or infiltration of the spermatic cord. The effectiveness of inguinal orchiectomy is probably related to denervation of the cord during dissection in the inguinal canal. In the series of Costabile et al. 80% of orchidectomized patients have persistent pain. Overall, the low rate of improvement of patients after the procedure and the mutilating and definitive nature of the orchiectomy should make the indication extremely cautious. It should be considered last, in patients clearly informed of the risk of persistent pain.
- Vasovasostomy improves symptoms in a small number of well-selected patients with chronic pain after vasectomy. Myers et al. report improved pain in 84%. Nangia et al. describe a complete disappearance of pain in nine out of 13 operated patients (69%). In relation to the epididymectomy, vasovasostomy can potentially restore fertility and not perform the permanent resection. Vasovasostomy was justified by the fact that post-vasectomy pain could be due to compression of cord nerve fibres by inflammatory granuloma associated with sperm extravasation. Excluding, the incidence of spermatic granuloma after vasectomy is of the order of 20 to 60%.
- Microsurgical denervation of the spermatic cord is rarely performed. The principle of microsurgical denervation consists in interrupting the sensory innervation of the testicle and epididymis at the level of the spermatic cord in the inguinal canal. This intervention requires a particular skill in microsurgery which makes it difficult to generalize.


