Dr. Marois is qualified to perform a no needle, no scalpel vasectomy, also known as a keyhole vasectomy, at his urology clinics in Greater Montreal and Quebec City.
Usually, the first step for patients seeking a vasectomy is to schedule an initial consultation. During this appointment, the patient fills out a short questionnaire, undergoes a physical examination and is given details about the procedure. Afterward, a second appointment is scheduled for the vasectomy. This take two separate appointments, and involved fees for consultation AND surgery.
Alternatively, patients can have both the initial exam and the vasectomy during a single appointment. However, this is only possible if the exam is normal and the patient does not have a bold disorder or has stopped taking blood thinners.
For your convince and preferences, we offer both possibilities.
Note that Dr. Marois will have to perform the vasectomy with two incisions if the patient is overweight, has a small scrotum, has a short vas deferens or has already had a surgery in his genital area (such as a vasovasostomy).
We recommend that the patient be accompanied by another person. When patients have someone with them, they can be offered medication if they begin to feel anxious.
Furthermore, we recommend that the patient avoid drinking coffee or taking any other stimulants on the morning of the vasectomy and that the patient wears tight- fitting underwear for better support.
Please note that the vasectomy procedure is performed in an unaffiliated private clinic and can’t be reimbursed through the Regie de l’assurance maladie du Québec (RAMQ). The confirmation of the patient’s sterility is sent by email after receipt of the results of the spermogram. If, in some rare cases, a second vasectomy should be necessary.
Please note that vasectomies are only performed in a disaffiliated private clinic and therefore not covered by the RAMQ. They are usually carried out in a single appointment. This includes consultation and infertility notification by email after reception of the spermogram’s results.
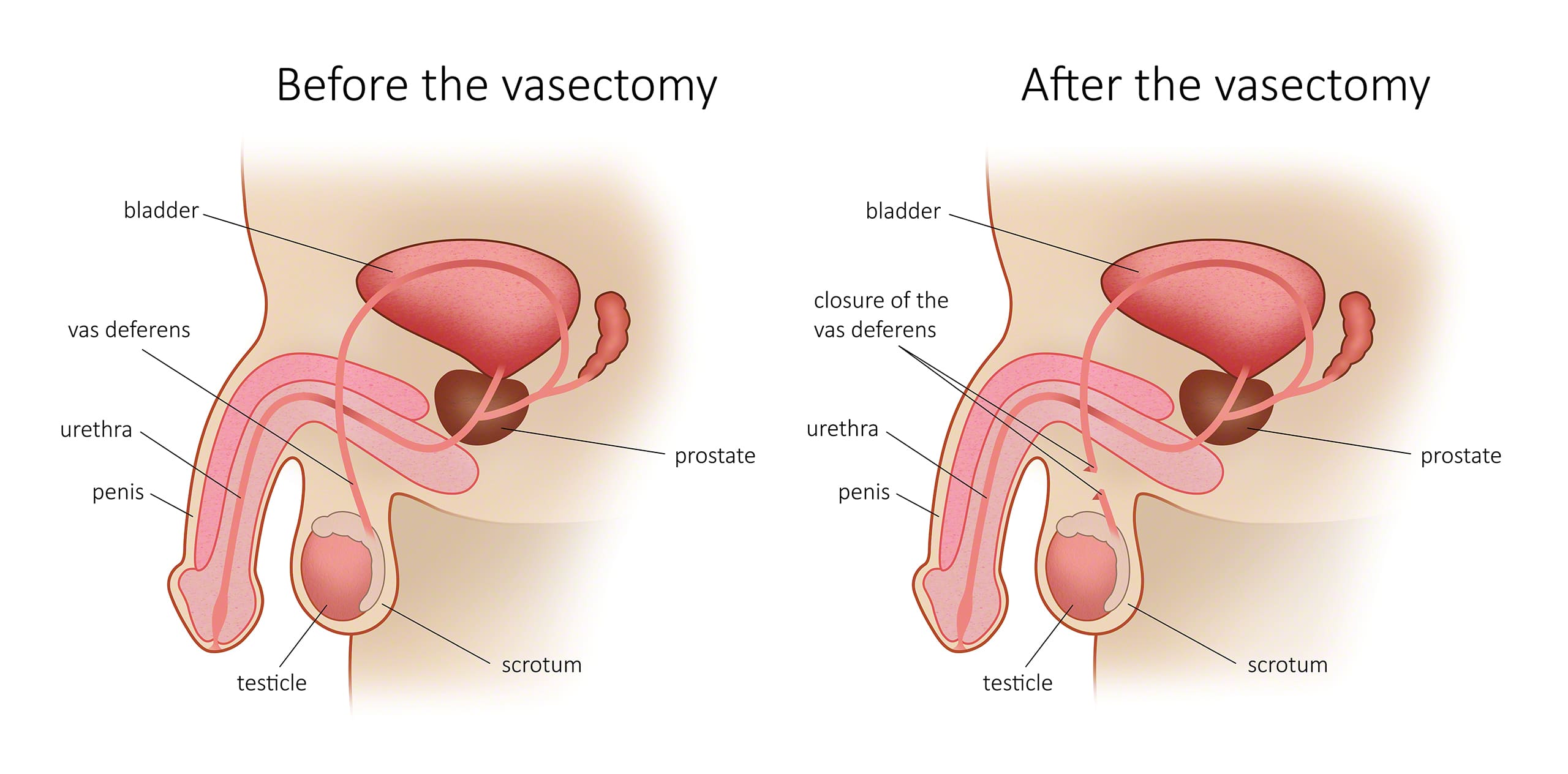
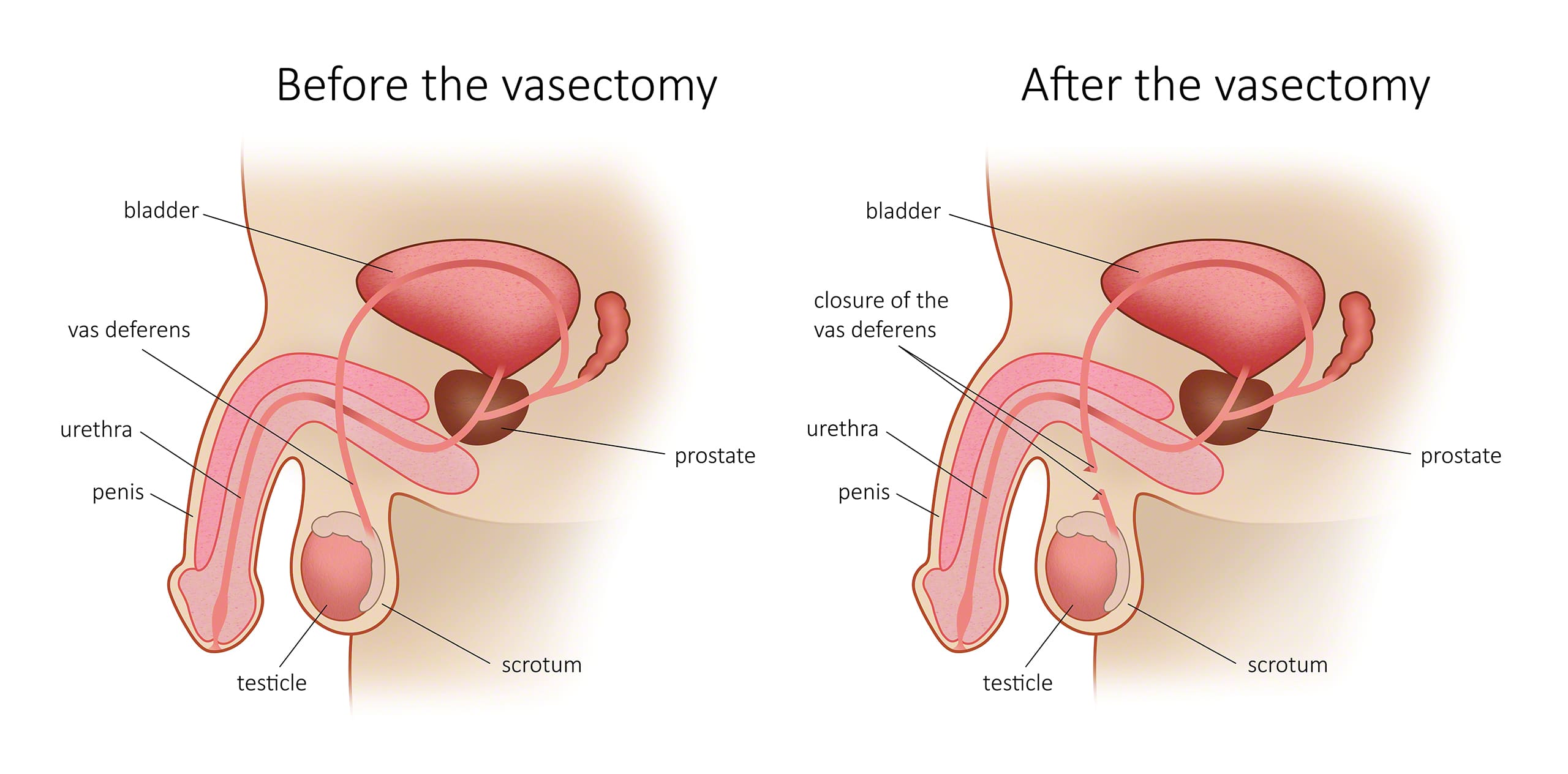
What happens during a vasectomy?
A no needle, no scalpel vasectomy involves several steps. First, Dr. Marois will hold the vas deferens in place using a clamp. Next, he will remove the vas so that it can be cauterized and ligated at either end.
Dr. Marois never uses metal clips to clamp the vas deferens. To minimize the risk of recanalization, Dr. Marois will isolate the vas deferens on the abdominal side by interposing spermatic fascia. This unique method takes a few minutes of extra work for each duct. It involves covering the vas deferens with a resorbable thread and a layer of tissue that encircles each duct.
Is a vasectomy a permanent method of contraception?
Are there potential complications to having a vasectomy?
Very rarely, the vas deferens grows back prior to the spermogram. This is known as early recanalization and occurs when the two ends of the canals reattach and allow the passage of spermatozoa (making the patient fertile).
Delayed spontaneous canalization, occurring after the vasectomy when the vas deferens has been cut, ligated and cauterized, is very rare.
Are there medical contraindications to a no needle, no scalpel vasectomy?
Does having a vasectomy influence your sex life?
Is the administration of the anesthetic painful?
However, the anesthetic is confined to the area around the injection and sometimes an unpleasant sensation can be faintly felt at the upper part of the vas deferens, in the abdomen.
There’s a small risk of hematoma, since the needle is inserted near veins. The surgery can begin 5 to 10 minutes after the anesthetic has been administered. Medication is offered to accompanied patients who are anxious about the procedure.
What technique is used for the vasectomy?
Men who are overweight, had scrotal surgery or been referred to the clinic following a failed vasectomy may require a vasectomy technique that involves two incisions (one on either side). This technique may also be necessary if the vas deferens are too short for a standard central incision. In such cases, the cost of the vasectomy is higher.
Can a spouse be present during the vasectomy?
The person who accompanies the patient to the procedure can be present in the operating room during the vasectomy if it helps to calm the patient. Note that a protective screen is placed over the patient’s chest to prevent him from seeing the surgery.
Contact us to schedule a no needle, no scalpel vasectomy in Montreal, Laval, on the South Shore or in Quebec City.


