Every day, an average of 58 men are diagnosed with prostate cancer. In addition to being the most common form of cancer in humans after skin cancer, it is the 3rd cause of cancer death in Canada.
Detecting prostate cancer at an early stage significantly increases the chances of successful treatment. Having a regular health exam and remaining alert to symptoms, is a good way to prevent and diagnose cancer as quickly as possible, if cancer exists.
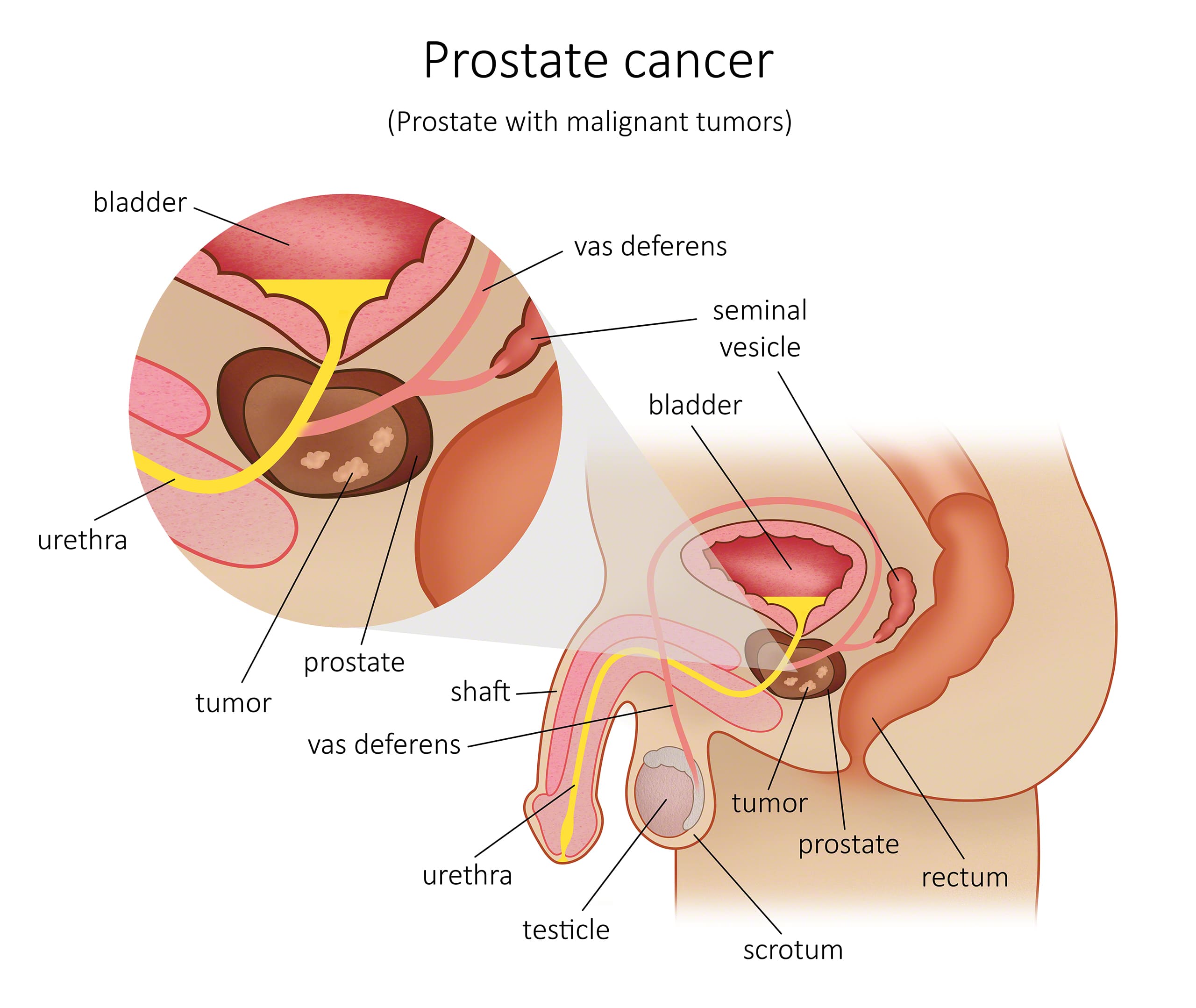
This cancer consists of a collection of cancer cells within the prostate, which can invade and destroy the tissues surrounding it. It can also spread (metastasize) to other parts of the body. This type of cancer usually grows slowly and can often be removed completely or treated successfully after being diagnosed.
What are the risk factors for prostate cancer?
While prostate cancer isn’t common among men under the age of 50, the risk of getting the disease increases as men get older. Prostate cancer is most often diagnosed in men over 65.
The incidence of prostate cancer is lower in men of Asian origin and higher in men of African origin. The latter are more likely to be diagnosed with the disease at a younger age than Caucasian men. They also tend to suffer more aggressive tumours and receive their diagnoses at a more advanced stage.
Family history and a diet rich in red meat are other predominant risk factors for prostate cancer.
Men with a family history of prostate cancer are at a higher risk for the disease and should speak to their doctor about developing a personalized screening program.
The incidence of prostate cancer is lower in men of Asian origin and higher in men of African origin. The latter are more likely to be diagnosed with the disease at a younger age than Caucasian men. They also tend to suffer more aggressive tumours and receive their diagnoses at a more advanced stage.
Family history and a diet rich in red meat are other predominant risk factors for prostate cancer.
Men with a family history of prostate cancer are at a higher risk for the disease and should speak to their doctor about developing a personalized screening program.
How is prostate cancer diagnosed?
- A digital rectal exam (DRE) is used to check the size and shape of the prostate to determine if there’s an abnormal area or mass.
- A prostate-specific antigen (PSA) test measures the level of PSA in the blood. PSA is a protein produced by the prostate gland and is what’s known as a tumour marker. A higher-than-normal PSA level is a sign of prostate cancer. However, high PSA levels are also associated with certain other non-cancerous prostate conditions, such as benign prostatic hyperplasia (BPH) or prostatitis.
- A transrectal ultrasound produces an image of the patient’s prostate gland using sound waves.
- A prostate biopsy may be performed if a digital rectal exam detects an abnormal area or mass, or if the PSA levels are higher than normal. The biopsy needle is injected through the perineal skin. Samples taken during a prostate biopsy are sent to a laboratory and a pathology report from the lab identifies whether or not cancer cells are present. Dr Marois combines this with MRI imagery: this technique enables Dr Marois to be more specific at collecting samples within the prostate.
- Magnetic resonance imaging (MRI) uses strong magnetic fields and radio waves to generate cross-sectional pictures of the body’s organs, tissues, bones and blood vessels. A computer turns the pictures into 3D images. Sometimes a dye known as a contrast material is injected into a vein before the test. This dye helps to accentuate the images. MRI tests are highly useful for detecting cancerous regions on the front side of the prostate that other tests might have missed. They may also be used in the event that the doctor suspects that cancer is present but the biopsy comes back negative. An MRI can also help the doctor guide the needle during the prostate biopsy.
- A bone scan uses radioactive material that attaches to the bones to produce an image of the skeleton. This test can be used to determine whether the prostate cancer has spread to the bones.
- A computed tomography scan (CT scan) is generally used to determine whether the cancer has spread beyond the prostate gland, in particular to the lymph nodes in the abdomen.
How is the stage of the prostate cancer determined?
The Gleason classification system is the most widely used tool for determining the stage
of cancer. Prostate tissue samples are examined under a microscope by a pathologist and assigned a grade of 1 to 5, depending on the pattern of the prostate cells.
The lower the pattern number, the more cancer cells appear, behave and arrange themselves like normal cells. Patterns 1 and 2 are seldom used, as these cells closely resemble normal cells in appearance. The pathologist assigns a grade corresponding to a pattern number for each cancer cell pattern present in the biopsy. Most prostate cancers have a Gleason pattern of 3, 4 or 5.
If the pathologist finds only two patterns of cancer cells, they will add their grades together to get the total Gleason score. For example, if they assign a grade of 3 to the predominant pattern of cancer cells and a grade of 4 to the next most common pattern, the Gleason score is 7. On the pathology report, this is typically written as 3+4=7/10.
The lower the pattern number, the more cancer cells appear, behave and arrange themselves like normal cells. Patterns 1 and 2 are seldom used, as these cells closely resemble normal cells in appearance. The pathologist assigns a grade corresponding to a pattern number for each cancer cell pattern present in the biopsy. Most prostate cancers have a Gleason pattern of 3, 4 or 5.
If the pathologist finds only two patterns of cancer cells, they will add their grades together to get the total Gleason score. For example, if they assign a grade of 3 to the predominant pattern of cancer cells and a grade of 4 to the next most common pattern, the Gleason score is 7. On the pathology report, this is typically written as 3+4=7/10.
What are the main treatments for prostate cancer?
There are a number of factors to consider when determining the appropriate prostate
cancer treatment for a patient. These include the type and stage of the cancer, the Gleason score, the patient’s symptoms. Additionally, the patient’s overall health, age, life expectancy and personal preferences are taken into consideration. The possible side effects of the treatment are also assessed.
Here are some of the medical treatment options for prostate cancer that may be offered following a diagnosis:
Rapid cancer testing at Dr. Marois’ clinics
Contact us to learn more about prostate cancer treatment options available to men in Greater Montreal and Quebec City.
Here are some of the medical treatment options for prostate cancer that may be offered following a diagnosis:
- Active surveillance Dr. Marois will closely monitor the patient to look for any signs and symptoms that the prostate cancer is progressing. The patient will come in for regular appointments and undergo tests every 3 to 6 months. If there are any signs that the prostate cancer is developing or spreading (this is known as disease progression), Dr. Marois will begin treating the patient.
- Radical prostatectomy This procedure involves the removal of the entire prostate gland, as well as some surrounding tissue, including the seminal vesicles. This is the most common type of surgery for treating prostate cancer. The procedure is most common among older patients but may also be recommended for younger patients with a high Gleason score.
- Radiation therapy Radiation therapy is a common prostate cancer treatment. Various techniques are used, including external radiotherapy, brachytherapy and systemic radiotherapy.
- Hormonal therapy Hormonal therapy is used most often for prostate cancer that has reached an advanced stage or that recurs (relapses) after other treatments have failed. This treatment can be administered in conjunction with radiation therapy.
- Chemotherapy Chemotherapy is used as a last resort for cases of advanced prostate cancer. In particular, it’s used to treat hormone-refractory prostate cancer: prostate cancer that doesn’t respond to hormone therapy or relapses after it. Among men with metastatic prostate cancer, chemotherapy is sometimes administered in conjunction with hormonal therapy.
Rapid cancer testing at Dr. Marois’ clinics
- Perineal prostate biopsy
- Prostate cancer screening
- Prostate ultrasound
Contact us to learn more about prostate cancer treatment options available to men in Greater Montreal and Quebec City.
Rapid cancer testing at Dr. Marois’ clinics
- Perineal prostate biopsy
- Screening Exams for Men
- Transrectal Prostate Ultrasound
- Rectal examination
- Prostate Specific Antigen (PSA)


